The Affordable Care Act
A comprehensive breakdown of the Affordable Care Act from an employer's perspective, including who qualifies and what they must do to comply.
Introduction
ACA. Affordable Care Act. Obamacare. It’s frequently a hot topic of discussion for political pundits, but for all that everyone seems to have heard of it and have differing views on the matter, there’s little public awareness or understanding of what the ACA actually means for employers.
This leaves businesses—especially smaller ones without robust HR departments—scrambling for information about how to remain in compliance with a complex set of rules that can have a major impact on how businesses operate.
What is the Affordable Care Act?
Passed in 2010 with the general goal of making healthcare more broadly available and affordable, the ACA includes a broad range of regulations and protections that impact healthcare providers, insurers, employers, and individual patients. Most of these have little to no impact on employers, including things like
-
The extension of parental insurance to young adults up to the age of 26
-
Protections for individuals with pre-existing medical conditions
-
Requiring insurance policies to completely cover preventative care such as cholesterol and depression screenings, vaccines, and smoking cessation programs
-
Ending yearly and lifetime limits on health benefits
Employers come into the ACA in several ways, but primarily in their role as providers of health benefits to their employees. At the most basic level, businesses with 50 or more full-time equivalent employees must offer appropriate health coverage to their employees and report this coverage or face a penalty. (We’ll talk about these requirements in detail in a bit.)
A Law in Flux
Since 2017, a number of changes have been made to the Affordable Care Act, and it is likely that changes will continue to be made in the coming years. Some parts of the act (such as protections for those with pre-existing conditions) enjoy bipartisan support and are unlikely to change.
Other, less popular parts (such as the individual mandate) are already out the door. Keeping an eye on ACA changes will be key to staying in compliance in a constantly shifting political climate.
Staying ACA Compliant
The Affordable Care Act has two major provisions that fall on many, but not all employers.
Staying ACA Compliant: Who Needs to Worry?
The Affordable Care Act has two major provisions that fall on many, but not all employers. These include the shared responsibility provisions and the employer information reporting provisions for offers of minimum essential coverage. These make up the bulk of employers’ responsibilities regarding the ACA. So how do you know whether they apply to you?
Are You an ALE?
The ACA term for a business that must be in compliance is an Applicable Large Employer or ALE. ALEs have 50 or more full-time equivalent employees. If you have well over 50 employees working full time and have for some time, this is easily translated: yes, you’re an ALE. If not, you’re not necessarily off the hook, as you’ll need to look more closely at what full-time “equivalence” means.
How to Calculate Your FTEs:
Know who NOT to count in these calculations:
-
Any employees who work from another country or a US territory do not count in this calculation, regardless of their citizenship status. ALE status is determined by looking only at the hours employees work in the 50 states or the District of Columbia.
-
Any employees who receive their healthcare through the military, whether that’s TRICARE or the VA, during the months that healthcare coverage is in effect
-
Any seasonal workers who are employed fewer than 120 days a year, if the employer qualifies for the Seasonal Worker Exception
-
Any volunteer employees working at nonprofit or governmental organizations
-
Work-study student employees. This specifically relates to those participating in federal or state work-study programs. Paid interns, on the other hand, do count as employees so must be included in these calculations.
Do the math:
Excepting those employees you’ve now removed from the question,
-
How many full-time employees do you have in a month? Full-time in this case means employees being paid for on average 30 or more hours a week or 130 or more hours a month. Each of these individuals counts as one FTE employee that month. Hang on to this number.
-
Taking into account all your employees who are paid for on average fewer than 30 hours a week (or 130 hours a month), total the number of hours these part-time employees were paid for that month, up to 120 hours each employee, then divide by 120. If the answer isn’t a whole number, round appropriately.
-
Add these two numbers together and you have your number of full-time equivalent employees that month.
-
But you’re not quite finished yet. Because businesses change sizes over time, ALE status is determined annually, based on the organization’s average size over the previous calendar year. So you’ll need to calculate your FTE for each month of the last year and divide by 12 (or the number of months you were in business last year). This is the number that you will use.
If this number is 50 or greater, you are considered an Applicable Large Employer. If not, you are currently exempt from these provisions of the Affordable Care Act. (If you’re getting close, though, it’s a good idea to start getting your ducks in a row now. The last thing you want is to pay a penalty because you procrastinated, or have to hold off hiring much-needed staff because you’re unprepared to provide appropriate benefits.)
New Businesses
If your business didn’t exist last year? You’ll need to make your best guess about how many people you reasonably plan to employ. More uncertainty, but less algebra. The IRS doesn’t seem to be interested in penalizing new businesses that make a good-faith effort to estimate hiring in their first year of operation.
Multiple Businesses with Common Ownership
There are some circumstances where these calculations may be different. If multiple businesses have the same ownership, for example, those business’ FTE employees should be combined when calculating whether they are an ALE.
Helpful Articles
Shared Responsibility Basics
If you’re an ALE, you’re on the hook for the ACA’s employer shared responsibility provisions.
Shared Responsibility Basics
If you’re an ALE, you’re on the hook for the ACA’s employer shared responsibility provisions. This means a few things:
-
You must offer minimum essential coverage for at least 95% of your full-time employees
-
This coverage must be affordable for your employees
-
It must provide at least minimum value to your employees and their dependents.
Alternately, you can pay a shared responsibility payment to the IRS (AKA a penalty tax). It’s not the best idea, but it’s legal and technically an available option.
Each of these has a specific legal meaning, so you shouldn’t ever be left wondering whether or not your coverage meets these requirements.
Minimum Value
A plan is said to provide minimum value if it covers at least 60% of the allowed cost of benefits that are expected to occur. This gets into a lot of complicated actuarial math, but for plans with standard features, the Center for Consumer Information and Insurance Oversight has an online calculator to determine whether it meets the minimum value requirements. Unusual plans with nonstandard features require actuarial certification to show that those features meet minimum value requirements.
Affordability
Affordability is formally defined as being no more than 9.5% of family income, adjusted for inflation. Luckily, you’re not expected to poll each of your employees about their household income and expenses to determine whether the health benefits you offer are affordable. There are three “safe harbors” that rely on information employers have readily available. Using any one of these to calculate affordability is acceptable. These are:
-
W-2 wages: If an employee’s required annual premium contribution is no more than 9.86% of their pay in 2019 (up from 9.56% in 2018) as reported in Box 1 of their current W-2, the coverage is considered affordable.
-
Rate of pay: Multiply an employee’s lowest hourly wage in a month by 130. If their required monthly premium contribution is no more than 9.86% of this number in 2019 (up from 9.56% in 2018), the coverage is affordable that month. (This method can’t be used for employees who work solely on commission.)
-
Federal poverty line: If the required employee monthly premium contribution for a month is no more than 9.86% in 2019 (up from 9.56% in 2018) of the federal poverty line for a single individual divided by 12, it is automatically considered affordable that month.
Offer
You know that you need to offer coverage, but you can’t just send out a text message stating that anyone who wants coverage should sign up tomorrow. There are rules regarding the offers themselves as well. These rules are pretty common-sense for anyone making a good-faith effort to allow their employees to enroll, but you should be aware of them nevertheless.
-
Eligible employees need to be offered coverage that begins within 90 days of their start date.
-
A plain-language summary of benefits must be provided before enrollment.
-
Employees cannot be threatened with firing or disciplinary action for signing up for coverage. (Yes, that’s obvious. Unfortunately, it still needed to be said.)
Shared Responsibility Payment
What happens if you aren’t in compliance? That’s where the shared responsibility payment comes in. The payment depends on the type of issue.
-
If you do not offer minimum essential coverage to 95% of your full-time employees: In this case, the penalty is $2000 per full-time employee, minus your first 30 employees. So if you have 50 full-time employees, the payment would be $2000 x (50-30), or $40,000. As you can see, this can get costly very quickly for larger organizations.
-
If you DO offer coverage to 95% of your full-time employees, but one or more employees still gets a premium tax credit on the Marketplace: This might happen either because the coverage is unaffordable or because they’re one of the <5% of your full-time employees who weren’t offered coverage. In these cases, the penalty is $3000 per employee who receives the tax credit.
Either of these payments is prorated per month the employees were not offered affordable coverage, so it’s better to get started late than to not offer the appropriate coverage all year.
All About Reporting
Reporting is the second major responsibility that ALEs have under the Affordable Care Act.
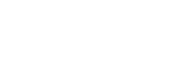
All About Reporting
Reporting is the second major responsibility that ALEs have under the Affordable Care Act. As an ALE, you must provide information to the IRS about the coverage offered (or not offered) to full-time employees, and also provide information to your covered employees. There are two forms for this purpose. (The IRS loves its forms.)
Form 1094-C is used to report your offers of coverage as a whole. It includes information about your business, whether your business is part of a larger ALE group, the number of employees in each month of the year, and whether minimum essential coverage was offered during that time.
Form 1095-C, on the other hand, is completed for each full-time employee and must also be furnished directly to them, in addition to being filed with the IRS. This is required regardless of whether the employee used the coverage and even when coverage was never offered.
Forms 1094-B and 1095-B are the employer’s responsibility only if self-insuring, meaning the company itself is covering the cost of healthcare for its employees, rather than using an outside insurer. In that case, though, the employer could still use the 1094-C and 1095-C as long as they include additional information regarding covered individuals.
If you are filing 250 or more information returns, you must do so electronically using the ACA Information Return system, or AIR. This is separate from the system used to file non-ACA documents such as 1099s, so don’t put it off, assuming that you already know how to e-file.
Deadlines
The general deadline for furnishing 1095-C to employees is January 31. In 2018, this was extended to March 2. As of this writing, there has been no indication whether deadlines will again be extended again in 2019.
Both 1094-C and 1095-C must be either postmarked by February 28 if using paper or filed by March 31 electronically.
Special Provisions for Small Businesses
Unlike larger businesses, you’re not required to provide health coverage for your employees. If you choose to, though, you have some additional options.
Special Provisions for Small Businesses
Not an ALE? This doesn’t mean the ACA doesn’t apply to you. In fact, some provisions of the Affordable Care Act apply specifically to businesses with fewer than 50 full-time equivalent employees.
SHOP
Unlike larger businesses, you’re not required to provide health coverage for your employees. If you choose to, though, you have some additional options. The Small Business Health Options Program (SHOP) is intended to help small businesses provide health insurance to their employees. Your organization can qualify for SHOP if you:
-
Have a primary business address in the state where you’re buying coverage
-
Have at least one employee enrolling who isn’t an owner or business partner or spouse of the owner. (Owners etc. can also enroll, provided that at least one employee does as well.)
-
Have between 1 and 50 FTE employees
-
Offer SHOP coverage to all of your full-time employees
If you enrolled in SHOP in 2017 or earlier, you did so through HealthCare.gov. From 2018 on, this is no longer an option. You have two options for enrolling in SHOP:
-
Enroll with your insurance company
-
Find an agent or broker who is authorized to sell SHOP insurance
Small Business Health Care Tax Credit
If you’re a small employer that offers health coverage to employees, you may qualify for a tax credit. Qualifying businesses are those that:
-
Have fewer than 25 FTE employees
-
Pay wages of less than $50,000 per FTE employee, adjusted for inflation. (This was $53,000 in 2017.)
-
Offer full-time employees a qualified plan through SHOP
-
Pay at least 50% of the cost of employee health coverage. (This doesn’t include spouses or dependents.)
The maximum credit is 50% of premiums paid for small business employers or 35% of premiums paid for small tax-exempt employers. The credit is available for two consecutive taxable years.
The amount of the credit itself is dependent on the size of the business. Generally speaking, the smaller the business, the more generous the credit. Form 8941 is used to determine the precise amount.
Helpful Articles
Get ACA Help
Remember, Complete Payroll has a dozen ACA Subject Matter Experts that can help your business get - and stay - compliant with this complex law.
Remember: they want you to succeed.
The purpose of the Affordable Care Act is to help Americans access healthcare. It’s true that the IRS can fine you for non-compliance, but they’d much rather you were successful in meeting the requirements. They’ve assembled YouTube videos and podcasts and multiple websites to help you do so.
Can it be overwhelming anyhow? Absolutely. But that doesn’t mean you have to do it alone. Sometimes bringing an expert in can give you just enough peace of mind to let you focus on the other important parts of keeping your business up and running smoothly. Does that sound like exactly what you’re looking for? Then get in touch with our ACA experts. Yes, it’s complicated. Let us make it easy.
Bahar Uttam
I have been working with Lacy Smart and her team for the last few years. I have been impressed by her responsiveness, accuracy, and high level of providing client satisfaction. She and her team are a wonderful testament to the organization!
Bonnie Deneef
I have worked with a few different payroll providers during my career. Complete Payroll is absolutely, by far, the most proficient and customer service-oriented provider I have been privileged to work with. Lindsay Ezard goes above and beyond to assist me with any question I may have. Thank You Lindsay!
Cathy Pace
Finger Lakes Wrestling Club Inc
We were referred to Complete Payroll years ago by a board member and haven't looked back since. When I first started working with them, I knew nothing about payroll. My first rep Lacey, and now JoAnn, are great to work with. Working with Complete Payroll has just been a wonderful all-around experience for me.
Christina Wagar
Dr. Christopher Mozrall
Complete Payroll is a great payroll company, and we love our CSR! She always has the answers to my questions without hesitation. There is very little (if any) wait time to get a call back.
Colleen Koll
The first suggestion I made after I joined Shear Ego was that if they were not yet using Complete Payroll, they should be. We continue to be impressed and happy with the quality and friendliness of service, and the excellent newsletters and up-to-date information on all things payroll and HR.
Debbie Klymkow
We moved to Complete Payroll about 3 years ago. It was seamless and working with Lacy Smart on Mondays is a breeze.
Dick Eakins
Norco Farms
Complete Payroll fits my budget, I never get bounced around between customer service reps, and it's very easy to enter my payroll. I simply take a photo of my payroll sheet and email it to my rep. There's never a problem! With them, it's business done, and business done right.
Don Cunningham
Complete Payroll Processing provided an easy transition from internal payroll processing. With payroll as their core competency, CP has the expertise to help mitigate errors and ease the burden of annual updates. Comprehensive reporting gives all the details needed and an organization can operate with an added piece of mind knowing that the payroll service is taken care of.
Eileen Reeves
After nearly 10 years, we are receiving the same or better service than when we started. The ability to reach our dedicated customer service representative in a timely manner is huge when there are deadlines in play. Requests for unique reports and integration with our other vendors has been handled without hesitation. We truly feel a partnership with Complete Payroll.
Emily Wyse
I just love Lindsay! She does an awesome job! She is very responsive and I like that she teaches me how to find things rather than just doing it for me.
Howard Clarke
H Clarke Services
We have been with Complete Payroll for quite awhile now and plan on staying. Thanks!
Watch Howard's Testimonial
John Worth
We have been well served by Complete Payroll. When we have needed support, it was given both in payroll and other employee matters, like handbooks.
Kelly Stephenson (former)
We have been using Complete Payroll for over five years and have found them to be responsive, professional, friendly, and cost effective. Customer service is best judged when something goes wrong. Complete Payroll is always there immediately to help fix the issue. Complete Payroll is a payroll partner, not just a payroll service.
Paul Cronk
I've been very pleased with the service and responsiveness of my CSR, and CP's continued dedication to provide us with all the tools we need to have a successful payroll and HR experience. You are always available when I have a question and always make sure that any problems that arise are worked through to my satisfaction.
Teresa Jackson
We have been customers for many years. Evolution Software is easy to use but, more importantly, Cindy is an email away and her knowledgeable, efficient, and quick to replies to our questions are appreciated. We're very happy with Complete Payroll.
Tina Canali
Complete Payroll is always there if we have a problem or need something special! Their response time is AWESOME!
Denni Harbaugh
My CSR, Andi Dimmick, is The Bomb! She's always friendly, cheery, and with all her clients, makes me feel like she has carved time out for ME. Her customer service is AWESOME, and the personal touch means so much!
Elvira Aletta
Everyone I talk to at CP is friendly and tries to help. If they don't have a ready answer, that's OK. They take the time to find one. Website is user friendly, too. The actual operation of payroll is dependable and reliable.
Peter Varlan
Things go quite smoothly and I have a very good rep: Megan!
Cindy Van Buren
Great customer support and service!
Lisa Lyons
Attica Auto Supply Inc
Friendly, answered all my questions, and never felt hurried.
Bonnie DeNeef
LeeAnn was just wonderful to work with.
Jackie Agusta
Lee Anne is a wonderful trainer. Concise and clear. A pleasure!!
Jennifer Pauly
The program has met our needs! Actually exceeded them!
Sue Budd
Great products, great people and no problems!
Gail Stowe
Stowe Potato Sales
Love working with Complete Payroll, especially with Joann Gaedeke. She is amazing! Very thorough and accurate; takes the pressure from me! Love it!
Nancy Miller
N&G Broadway Inc
Very friendly staff, and you are always on top of the services you offer.
Chris Smith
I appreciate updates that Complete Payroll provides. Site is easy to navigate. Our rep, Karla, is so accommodating and friendly. We appreciate her also. So happy we made the switch to Complete Payroll!
Frances Sweeney
The service that we have received has been EXCELLENT and I can't say enough about Lindsay Ezard's patience and support. Everyone that I have had contact with is professional, knowledgeable, and personable. I have received many calls from your competitors wanting to talk to us but I tell them I am very happy with our service!
Lora Miller
Great company to work with. Wonderful people; knowledgeable, helpful, and friendly!
Helen Cunningham
Customer Service and payroll representatives are excellent!
Sally Kovatch
The program works very well for our company. We like the virtual payroll option and our Account Representative, Ashley, is always very responsive and helpful!
Teri Peters
For 11+ years, Andrea Dimmick has been our CSR. She is extremely competent, helpful, responsive. Evolution portal, once trained, is easy to use and again, if we ever run into an issue, Andrea walks us right through. I would highly recommend... and have!
Nicole Begin
Love working with CPP. They have made life so much simpler for me.
Mary Sutter
I have worked with two other payroll companies and Complete Payroll has been the best in payroll custom packages and customer support! The payroll reports are readable with larger font when printed and program is user friendly.
Laura Lane
The customer service is beyond compare!
Barbie Gozelski
LeRoy Country Club
When I need something, you always help. You're easy to get ahold of; you DON’T put me on hold! I get to email or talk to a real person (Lindsay) and she's always consistent.
Nancy Miller
N&G Broadway Inc
Very friendly staff, and you are always on top of the services you offer!
Patricia Gilbertson
CPP has resources that consistently monitor payroll regulations at all levels that ensures compliance. This is a great boon for a small business with limited personnel.
Elizabeth Barefoot
I have recommended Complete Payroll to my clients for years. You have the best customer service of any payroll company I deal with. I know that mistakes will happen on occasion, but Complete Payroll really works to resolve issues promptly.
Kris Dussmann
We are a Complete Payroll customer and have been very happy with our relationship. We have had no problem referring CPP to our business owner clients.
Margaret Urlacher
Pittsford Realty Corp
Customer Service is awesome! Love Andrea 😀
Liz Maher
Our payroll specialist, Ashlee Adams, is extremely knowledgeable, helpful and quick to respond to all questions and concerns. She has alleviated many stressful situations for our company and is a true pleasure to work with! Thank you Ashlee!
Marybeth Simoneit
Friendly employees, lots of resources.
Kathy Cassetta
You have the best employees working for you. They are professional and a delight to work with!
Joe Czerny
Service reps are so helpful and always available. Andrea is the best!
Mark Logan
I love our CSR Megan. She makes my life so easy. I used to be with one of your competitors and the CSR there treated me like a number. Megan treats me like she is part of my team.
Patty Dugan
Any time I need anything we always have a prompt response from you.
Kris Dussmann
We are a Complete Payroll customer and have been very happy with our relationship. We have had no problem referring CPP to our business owner clients.
Debbie Blacklock
Fantastic service! Friendly helpful staff. Your company was and is the most sourced not only with payroll needs but also with the update and verbal connection with your clients when it came to the COVID-19 PPP. Believe me when I tell you, I had less help from my bank or my Accountant! Thank you!
Recent Articles from the Blog
We're constantly publishing content about payroll, human resources or anything related to managing your people.
Subscribe to Our Newsletter
Twice a month we share relevant and timely blog articles and other resources. No solicitations. No funny business. Just quality stuff to help employers.